By Simon DuBois, Psychologist
By Simon DuBois, Psychologist
It’s a proud and exciting moment for us at The Health Lodge as we celebrate the publication of our first research paper!
Since our inception, we’ve held a strong commitment to providing healthcare that honours the full complexity of people’s wellbeing. This commitment has been guided by the integrative healthcare model, which brings together the best of conventional and complementary medicine in a collaborative, patient-centred framework.
But how do we know we are applying this model effectively and that it’s really serving our patients? How do we ensure that our care is genuinely responding to the needs and expectations of the people we serve? And just as importantly, how do we continue improving?
These are the questions that inspired us to collaborate with Dr Matthew J Leach, a leading Australian health services researcher, registered nurse, and naturopath. Dr Leach has a longstanding interest in the development and evaluation of models of care that address the real-world complexity of health and healing. Together, we embarked on a research journey to better understand the experience of integrative care, not just from the perspective of practitioners (our second research paper not far from publication), but more crucially, from the experiences of our patients.
Why Patient Experience Matters
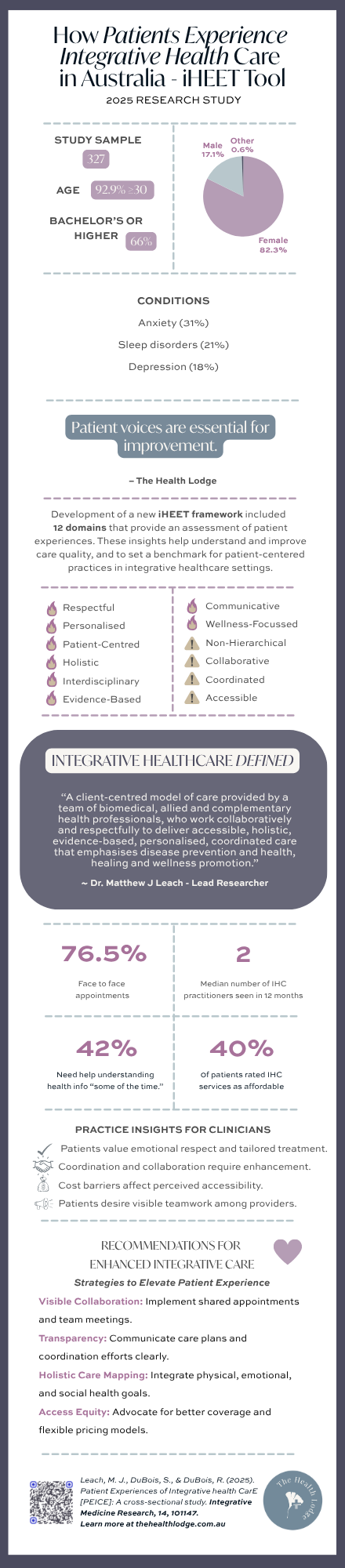
Although both practitioner and patient interest in integrative healthcare (IHC) has grown significantly over recent decades, the actual experience of patients navigating this model has remained largely unexplored. This gap in the literature is particularly important because IHC, by design, places the patient at the centre of care. It emphasises collaboration, respect, personalisation, and a whole-person view of health. In a landscape shaped by more informed and empowered consumers, integrative healthcare is emerging as a model well-suited to contemporary needs.
As defined by Dr Leach, integrative healthcare is “a client-centred model of care provided by a team of biomedical, allied and complementary health professionals, who work collaboratively and respectfully to deliver accessible, holistic, evidence-based, personalised, coordinated care that emphasises disease prevention and health, healing and wellness promotion.”
Despite its growing popularity, the question remains: is this how integrative care is actually being experienced by patients?
What We Did
With the leadership and guidance of Dr Leach, we participated in a national study examining the patient experience of integrative healthcare. This was a rare and valuable opportunity for our integrative medical centre clinic along with several others to contribute to the evidence base around a model we deeply believe in.
Using the newly developed Integrative Healthcare Experience Tool (iHEET), the study surveyed over 300 individuals who had accessed care at various integrative health centres around Australia in the previous 12 months. The aim was to explore the extent to which patients experienced the core principles of IHC in real-world practice. These twelve principles included:
- Respectful
- Personalised
- Patient-centred
- Holistic
- Non-hierarchical
- Interdisciplinary
- Collaborative
- Coordinated
- Evidence-based
- Accessible
- Communicative
- Wellness-focussed
What We Learned
Encouragingly, the results revealed an overwhelmingly positive experience of integrative healthcare across patients. The majority reported that their care aligned closely with the intended principles of IHC. Notably, men—who are often underrepresented in healthcare research, reported particularly positive outcomes, which challenges some assumptions about gender and help-seeking in healthcare environments.
Yet the research didn’t shy away from the areas that still need attention. Participants noted that while collaboration between providers often occurred behind the scenes, it wasn’t always visible to the patient. Increasing the transparency of interdisciplinary teamwork is one area where integrative practices can grow. Accessibility also emerged as a key challenge, both geographically and financially, which points to the broader need for systemic support to make integrative care more equitable and available to all. With respect to this issue we have been seeking and awarded a grant from the Primary Health Network to provide support in this area of need, and will continue to keep our eyes open for more grant opportunities to subsidise the health care we deliver.
Why It Matters
This study is the first of its kind to explore patient experiences of integrative healthcare in Australia. The findings have reinforced our belief in the value of the integrative model, not just as an idealistic theory, but as a lived and effective reality for patients. At the same time, we are reminded of our responsibility to continually listen, evolve, and improve.
Healthcare must remain responsive, and that means being guided not only by clinical expertise and research, but by the lived experience of those receiving care. As a team, we feel newly energised to continue refining our approach, making our collaborations more visible, improving access for a broader range of people, and deepening the integrity with which we practice integrative care.
Looking Ahead
To those of you who already entrust us with your care, thank you. And if you’re seeking a model of healthcare that values you as a whole person, and brings together a thoughtful team of practitioners to walk beside you, please get in contact.
And if you are interested, you can access the research paper in full here: https://doi.org/10.1016/j.imr.2025.101147